How EpiSwitch® Blood Markers Advance Precision Medicine and Cancer Care
Category: EpiSwitch®
Read Time: 6 Minutes
Category: EpiSwitch®
Read Time: 6 Minutes
Last updated: 16 June 2023
Precision medicine is a term that is frequently over-used and frankly, abused today. Often, what is referred to as precision medicine is no more than defining a smaller group of individuals using broad shared characteristics, but without truly precise targeting using personalized traits. In the context of cancer treatment, patients with the same diagnosis are often recommended the same course of treatment. Unfortunately, this disregards the fact that many therapies may be more effective for some patients than others, and consequently, each patient's treatment journey may differ significantly. Adopting a one-size-fits-all approach leads to many patients being prescribed medicines that do not work for them and may trigger harmful side effects. Particularly with cancer drugs, these side effects can develop quickly, often be quite serious, and create uncertainty around whether to permanently discontinue treatment or recommend a temporary pause to reset the patient's health.
The healthcare industry is striving to do better. Doctors have a few tests they can order to help guide a treatment plan for their patients. Healthcare insurers also have a vested interest in these tests, aiming to provide the best care to patients while efficiently using their funds, which is especially important given today's expensive blockbuster drugs. As we'll see below, the tests and therapies commonly referred to as “precise” often cast a broad net around the disease populations. It is important to acknowledge this limitation and continue striving for more targeted and individualized approaches in healthcare.
Top of this list is the latest class of cancer-fighting therapies – called immune checkpoint inhibitors (ICIs) – which in some cases, can offer a real hope of durable disease control for some cancers. They harness a person's immune system to find and fight their tumor and can even lead to complete recovery. Checkpoint inhibitors have transformed oncology treatment, especially in advanced-stage cancers that are harder to treat.
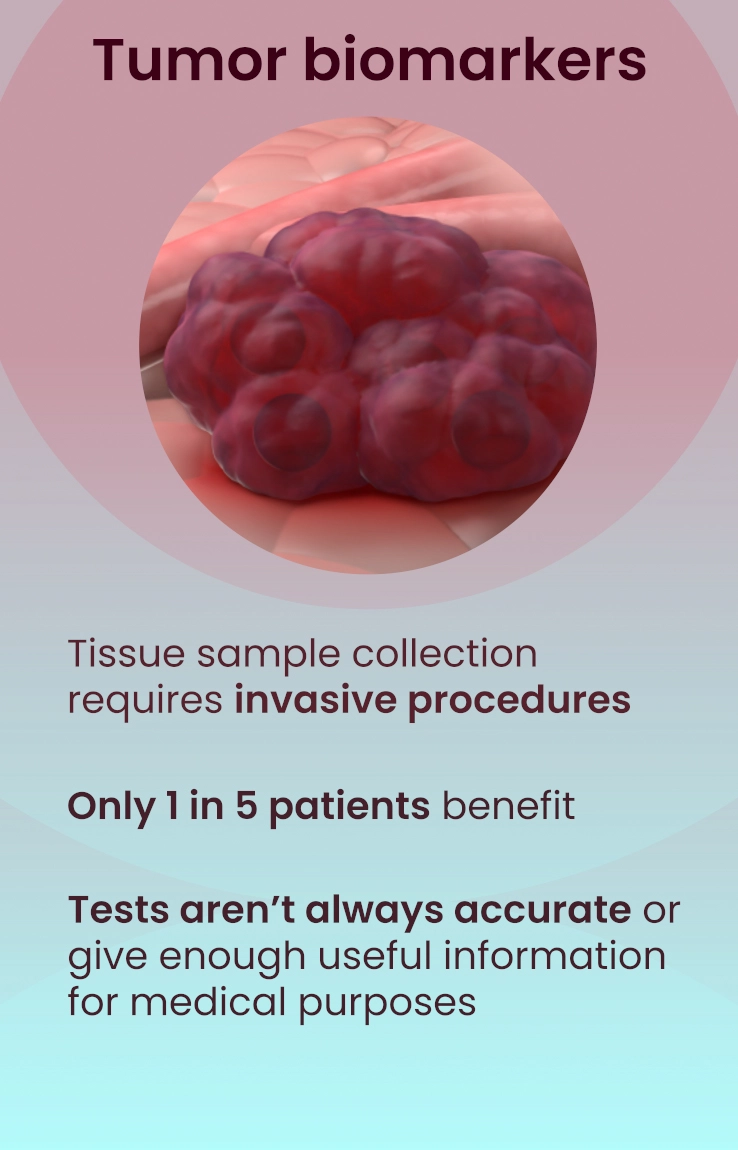
Sadly, checkpoint inhibitors typically only benefit 1 in 5 patients. Ideally, doctors would be able to identify and treat only those individuals who would respond positively, while sparing other patients from unwarranted side effects. Yet the tests currently available to and relied upon by doctors do NOT predict, with any accuracy, how a patient's cancer will respond to this medication.
There is a scenario where a cancer patient visits their doctor and gets a routine blood test. The test measures molecular signals in the blood that are unique to that individual. This is used to provide clear, valuable information informing the doctor of the likelihood that an ICI would benefit the patient.
Equipped with this knowledge, the doctor and patient can confidently decide on a personalized treatment plan that carries a higher chance for an enduring health benefit. Now we have a personalized, precise result for each patient – precision medicine realized.
The appeal of a smart blood test that accurately helps us to make an informed decision about cancer therapy is clear. But how can a test that uses blood outperform standard tests that directly look at a tumor sample—the focal point of the disease?
We often label cancer based on the organ in which it originates, such as lung cancer or breast cancer, but tumors with the same diagnosis can have vastly different biology.
Why cancer does or doesn't respond to checkpoint inhibitors is a challenging problem to solve. This response depends on a complex interplay of various factors, including between tumor cells themselves, the surrounding tissue, the individual's immune system, their metabolism, and more.
Effectively answering important questions about cancer and choosing the most beneficial treatment options is sometimes very difficult to achieve, especially when only relying on a tumor biopsy which gives an incomplete picture of these other elements.
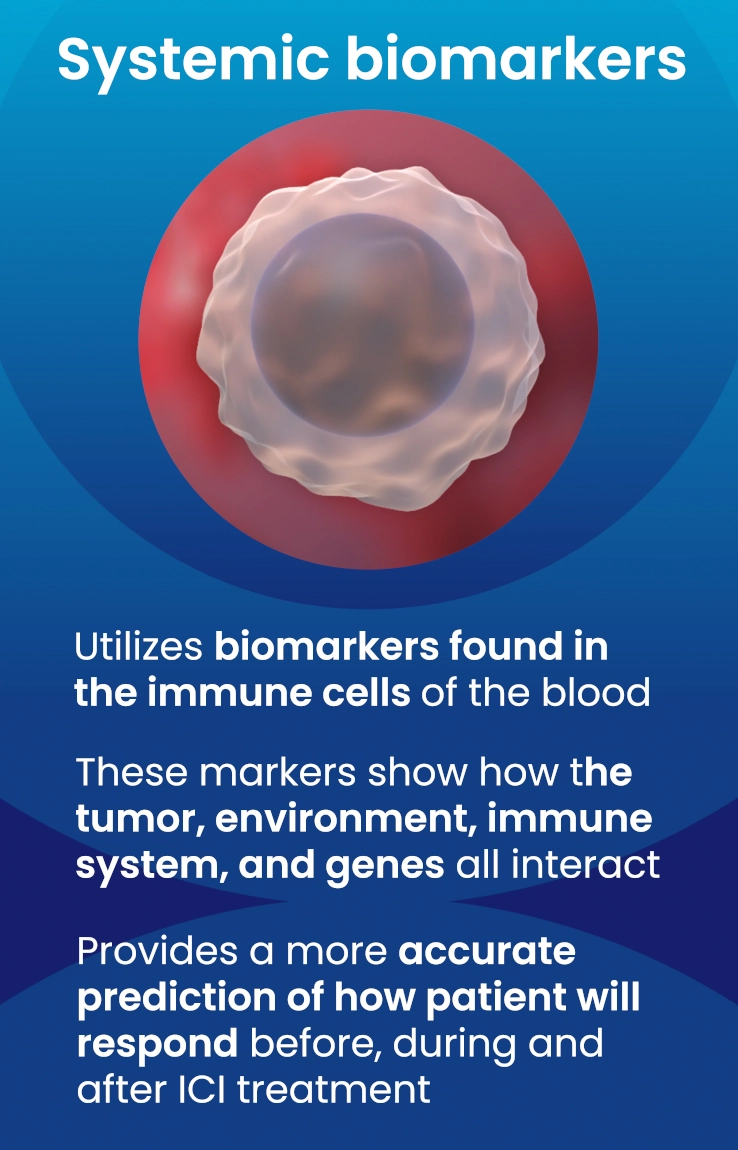
EpiSwitch testing looks mainly within white blood cells that travel the body looking for signs of disease and alerting the immune system. EpiSwitch is unique because it measures treatment-related data from a cancer patient's blood cells.
Our DNA contains the instructions for creating all the machinery our body needs to live. The genome is our library of these DNA instructions that help organize and regulate our cells and our body's needs to support survival.
This elaborate system is responsible for creating us and enables everything we are capable of doing. Changes in this system, combined with environmental and metabolic influences, alter the organization and regulation of our genome, which can lead to significant effects on our health.
Traditional clinical tests typically look at one aspect of this biological system, for example, mutations present in the linear DNA strands, consisting of A, C, T and G nucleotides. It turns out, to get the meters of DNA that make up the chromosomes into an individual cell, requires quite a bit of organization. This involves packaging the DNA into a dense three-dimensional structure, resembling a sphere, which is replicated every time a cell divides.
Loading...
EpiSwitch tests, such the flagship CiRT (Checkpoint inhibitor Response Test), are designed to measure this powerful, purposeful organization within cells—3D genomics—that combines information across all layers of genomic control, bringing together information about a person's genetic risks, changes in gene expression, and environmental or metabolic influences.
EpiSwitch 3D genomic tests can predict patient outcomes accurately because of their ability to capture multilayered information across the body. The technology makes it straightforward to discover and measure stable 3D genomic patterns shared between patients with similar outcomes, such as their response to a drug. As a result, it is now possible to routinely build practical and robust clinical tests using the same process that delivered EpiSwitch CiRT.
EpiSwitch CiRT is the only blood test that predicts a patient's most likely response to immune checkpoint inhibitor (ICI) therapies. The test provides actionable information to help guide optimized treatment decisions, including the potential use of ICI therapies. At the time of writing this article, EpiSwitch CiRT is available to registered physicians in the US and UK. For more information on CiRT, visit myCiRT.com.
Oxford BioDynamics is committed to advancing personalized healthcare by continuing to use the EpiSwitch platform to develop and commercialize precision medicine tests for life-changing diseases. For exciting new applications of our technology, please follow us on social media and subscribe to our blog by joining our mailing list.
Subscribe to receive our latest blog posts
Topics from groundbreaking discoveries to cutting-edge advancements and industry
trends.
A first-of-its-kind blood test to provide guidance on navigating the toughest challenges associated with use of an essential, widely-used class of cancer therapies: Immune Checkpoint Inhibitors.
Now every patient can benefit from the world’s first test to predict how a patient will respond to immune checkpoint inhibitor therapy with high accuracy.
Learn About CiRT